PLANTAR FASCIITIS / HEEL PAIN

Muscle Activation Technique
July 10, 2016
Your Journey to ACL recovery
September 7, 2016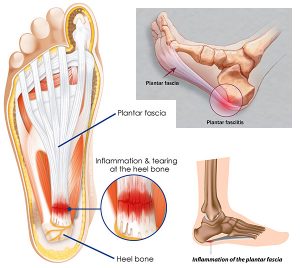 Plantar fasciitis is caused by drastic or sudden increases in mileage, poor foot structure, and inappropriate running shoes, which can overload the plantar fascia, the connective tissue that runs from the heel to the base of the toes. The plantar fascia may look like a series of fat rubber bands, but it’s made of collagen, a rigid protein that’s not very stretchy. The stress of overuse, overpronation, or overused shoes can rip tiny tears in it, causing pain and inflammation, a.k.a. plantar fasciitis.
Plantar fasciitis is caused by drastic or sudden increases in mileage, poor foot structure, and inappropriate running shoes, which can overload the plantar fascia, the connective tissue that runs from the heel to the base of the toes. The plantar fascia may look like a series of fat rubber bands, but it’s made of collagen, a rigid protein that’s not very stretchy. The stress of overuse, overpronation, or overused shoes can rip tiny tears in it, causing pain and inflammation, a.k.a. plantar fasciitis.
Causes:
You’re at a greater risk of developing plantar fasciitis if you’re overweight or obese. This is due to the increased pressure on your plantar fascia ligaments, especially if you have sudden weight gain. Women who are pregnant often experience bouts of plantar fasciitis, particularly during late pregnancy.
If you’re a long-distance runner, you may be more likely to develop plantar fascia problems. You’re also at risk if you have a very active job that involves being on your feet often, such as a factory worker or a restaurant server. Active men and women between the ages of 40 and 70 are at the highest risk for developing plantar fasciitis. It’s also slightly more common in women than men.
If you have foot problems, such as very high arches or very flat feet, you may develop plantar fasciitis. Tight Achilles tendons, which are the tendons attaching your calf muscles to your heels, may also result in plantar fascia pain. Simply wearing shoes with soft soles and poor arch support can also result in plantar fasciitis.
Plantar fasciitis isn’t typically the result of heel spurs. A heel spur is a hook of bone that can form on the heel bone, or calcaneus, of the foot. According to the American Association of Orthopedic Surgeons (AAOS), one out of every 10 people has a heel spur, but only one out of 20 people with heel spurs experience pain.
Symptoms:
Symptoms of plantar fasciitis consist of a gradual onset of pain under the heel which may radiate forwards into the foot (foot arch pain). There may be tenderness under the sole of the foot and on the inside of the heel when pressing in. The pain can range from being slightly uncomfortable to very painful depending on how badly it is damaged.
Pain is usually worse first in the morning because the foot has been in a relaxed position all night and the plantar fascia temporarily shortens. After walking around this usually eases as the tissues warm up and gradually stretch out. When the condition is present, similar periods of moving around following inactivity such as sitting for long periods can also trigger the pain.
Plantar Fasciitis Treatment:
The good news is that plantar fasciitis is reversible and very successfully treated. About 90 percent of people with plantar fasciitis improve significantly within two months of initial treatment.
If your plantar fasciitis continues after a few months of conservative treatment, your doctor may inject your heel with steroidal anti-inflammatory medications (corticosteroid). Cortisone injections have been shown to have short-term benefits but they actually retard your progress in the medium to long-term, which usually means that you will suffer recurrent bouts for longer.
Due to poor foot biomechanics being the primary cause of your plantar fasciitis it is vital to thoroughly assess and correct your foot and leg biomechanics to prevent future plantar fasciitis episodes or the development of a heel spur.
Your physiotherapist is an expert in foot assessment and its dynamic biomechanical correction. They may recommend that you seek the advice of a podiatrist, who is an expert in the prescription on passive foot devices such as orthotics.
Phase 1 – Early Injury Protection: Pain Relief & Anti-inflammatory Tips
As with most soft tissue injuries the initial treatment is Rest, Ice, and Protection.
In the early phase you’ll most likely be unable to walk pain-free. Our first aim is to provide you with some active rest from pain-provoking foot postures. This means that you should stop doing any movement or activity that provoked your foot pain in the first place.
Ice is a simple and effective modality to reduce your pain and swelling. Apply for 20-30 minutes each 2 to 4 hours during the initial phase or when you notice that your injury is warm or hot. A frozen water bottle can provide you with an ice foot roller that can simultaneously provide you with some gentle plantar fascia massage.
Anti-inflammatory medication (if tolerated) and natural substances arnica may help reduce your pain and swelling. However, it is best to avoid anti-inflammatory drugs during the initial 48 to 72 hours when they may encourage additional bleeding. Most people can tolerate paracetamol as a pain reducing medication.
To support and protect your plantar fascia, you may need to be wear a plantar fascia brace, heel cups or have your foot taped to provide pain relief. As mentioned earlier, the cause of your plantar fasciitis will determine what works best for you. Your physiotherapist will guide you.
Your physiotherapist will guide you and utilize a range of pain relieving techniques including joint mobilizations for stiff joints, massage, electrotherapy, acupuncture or dry needling to assist you during this pain-full phase.
 Phase 2: Regain Full Range of Motion
Phase 2: Regain Full Range of Motion
If you protect your injured plantar fascia appropriately the injured tissues will heal. Inflamed structures will settle when protected from additional damage, which can help you avoid long-standing degenerative changes.
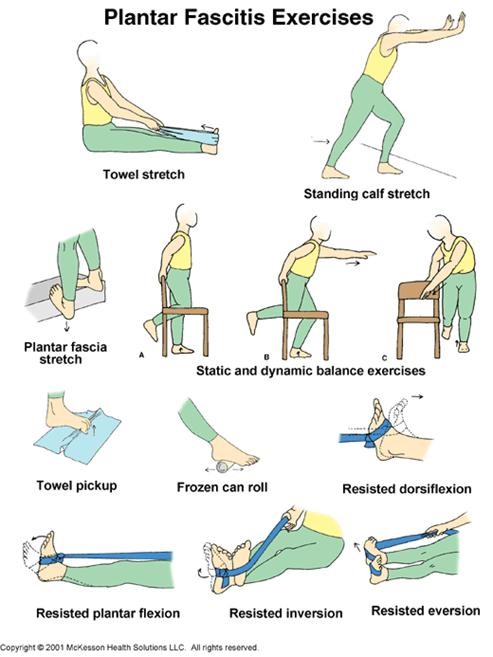
Plantar fasciitis may take from several weeks (through to many months) to heal while we await Mother Nature to form and mature the new scar tissue, which takes at least six weeks. During this time period you should be aiming to optimally remold your scar tissue to prevent a poorly formed scar that may become lumpy or potentially re-tear in the future. It is important to lengthen and orientate your healing scar tissue via massage, gentle stretches, and light active exercises.
In most cases, your physiotherapist will identify stiff joints within your foot and ankle complex that they will need to loosen to help you avoid plantar fascia overstress. A sign that you may have a stiff ankle joint can be a limited range of ankle bend during a squat maneuver. Your physiotherapist will guide you.
Phase 3: Restore Foot Arch Muscle Control
Your foot arch is dynamically controlled via important foot arch muscles, which be weak or have poor endurance. These foot muscles have a vital role as the main dynamically stable base for your foot and prevent excessive loading through your plantar fascia.
Any deficiencies will be an important component of your rehabilitation. Your physiotherapist is an expert in the assessment and correction of your dynamic foot control. They will be able to help you to correct your normal foot biomechanics and provide you with foot stabilization exercises if necessary.
Phase 4: Restore Normal Calf & Leg Muscle Control
You may find it difficult to comprehend, but all of your leg (calf, thigh and hip) muscles play an important role in controlling your foot arch and its normal function. Your physiotherapist will assess your leg muscle function and provide you with the necessary treatment or exercises as required.
 Phase 5: Restore Normal Foot Biomechanics
Phase 5: Restore Normal Foot Biomechanics
Your foot biomechanics are the main predisposing factor to plantar fasciitis. After a biomechanical assessment you may be recommended a soft orthotic or a custom made orthotic prescribed by a podiatrist.
Phase 6: Improve Your Running and Landing Technique
If your plantar fasciitis has been caused by sport it is usually during repetitive activities, which place enormous forces on your plantar fascia.
In order to prevent a recurrence as you return to sport, your physiotherapist will guide you with technique correction and exercises to address these important components of rehabilitation to both prevent a recurrence and improve your sporting performance.
Depending on what your sport or lifestyle entails, a speed, agility, proprioception and power program will be customized to prepares you for light sport-specific training.
Phase 7: Return to Sport or Work
Depending on the demands of your chosen sport or your job, you will require specific sport-specific or work-specific exercises and a progressed training regime to enable a safe and injury-free return to your chosen sport or employment.
Your physiotherapist will discuss your goals, time frames and training schedules with you to optimize you for a complete return to sport or work. Work-related injuries will often require a discussion between your doctor, rehabilitation counsellor or employer.
Phase 8: Footwear Analysis
Often it is poorly designed footwear that can predispose to the injury. Seek the professional advice of your healthcare practitioner.
To be successful at treating plantar fasciitis, you will need to:
- Be patient and consistent. The majority of cases of plantar fasciitis go away in time if you regularly stretch, wear good shoes, and rest your feet so they can heal.
- Start treatment right away. Don’t just ignore the pain and hope it will go away. The longer you wait to begin treatment, the longer it will take for your feet to stop hurting.
Pablo.




